As I write this introduction to the latest edition of the Hempsons Social Care Newsbrief, the sector can be forgiven for feeling a little sorry for itself. Turmoil in government, a cost of living crisis and record numbers of people leaving the social care sector do not make for easy reading. We therefore aim to give you top tips and legal updates to help lighten the load and remind you of our ever present team of lawyers on hand to give you initially free advice when you need it, to support you through difficult times.
This edition sees articles across a range of themes. You’ll hear from me around the new CQC inspection regime, together with reminders on duty of candour and Reg 12 safe care and treatment – neither of which have changed but are always a hot topic and something CQC look closely at.
Rachael Hawkin, associate in my team, takes you through when you might find yourself or your service involved with the Court of Protection. Julia Gray, associate in employment, explores whistle-blower protection and Faisal Dhalla, who heads up our care homes corporate team, sets out some tips for anyone looking at exiting the market or acquiring a new service.
We are delighted to have an exclusive interview with Nick Swash, chief executive of the Independent Care Group, who gives us his thoughts on his first year being involved with the sector and in particular finding ways to unite multiple small and medium sized businesses to have a voice together.
Finally, for the second year in a row Hempsons are delighted to have won the ‘Legal & Professional & Business Services’ at the Care Sector Supplier Awards on 25 November 2022.
I hope there is something for everyone in this edition and please get in touch if you have any questions or comments.
In July 2022, CQC formally confirmed the arrangements for its new inspection regime, including in particular the release of the new Key Questions and Quality Statements that will form the basis of a new points scoring system that will inform ratings going forward.
CQC describe quality statements as:
Commitments that providers, commissioners and system leaders should live up to. Expressed as “we statements”, they show what is needed to deliver high quality, person centred care.
But how will the new inspection regime work?
Quality statements will focus on specific topic areas under key questions. These will set clear expectations of providers, based on people’s experiences and the standard of care expected. They will replace the publication ‘Key Lines of Enquiry, prompts and ratings characteristics‘.
There will be six evidence categories to organise information under statements and this will move from over 300 Key Lines Of Enquiry to 34 quality statements.
Assessments will no longer be tied to set dates or be driven by a particular rating, but instead CQC will use “soft intelligence” to decide which services they need to physically visit (“cross the threshold”). Inspectors will spend more time observing care and talking to staff and people who use services and will produce shorter and simpler reports, showing more up to date assessments.
Of course, there will still be an evidence gathering stage, but that will likely take place in advance (to inform the visit), rather than taking up a large proportion of the visit.
In person visits will only occur where there is a clear need to do so – so that might mean more frequent visits where continuous monitoring is required but should also mean that ratings given are more meaningful and actually represent the current position on the ground and not that from two or three years ago. It should hopefully also address the current lacuna faced by those services rated “requires improvement” – who are not bad enough to need six monthly re-inspections, but then don’t get the opportunity to showcase how they have improved and might now be rated as “good”.
The timetable for the new regime was originally supposed to start in summer/autumn 2022 with early adopters enlisted from October, and the plan for a full role out in January 2023. However, recent information from CQC (in December 2022) was that adjustments are being made already, as a result of feedback from those involved in the process, so the timetable for full roll out has been paused. Implementation is now not expected until much later in 2023, possibly as late as the Autumn so keep an eye on CQC website for details.
Watch this space for when the new regime will actually start, but know that it’s coming and any variation from the currently laid out plans, is likely to be minimal.
CQC have a helpful webinar which walks you through the process – worth a watch at only 31 minutes long!

There will be six evidence categories that will set out exactly what information needs to be collected.
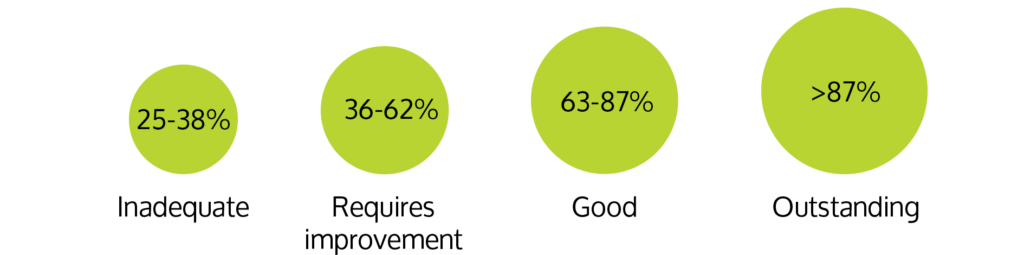
The quality of that evidence will then be rated 1 – 4, to then give an average percentage and an overall rating:
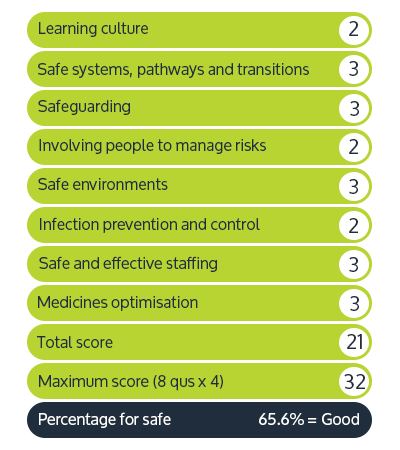
Example scoring therefore might look like this:
Safe key question:
This will be a combination of:
- observation (of care and the care environment)
- people’s experience of the service
- staff and leaders
- partners
- outcomes
- processes
A sample annual process therefore might look like this:
- relationship management call
- evidence submitted via provider portal
- review evidence and assess against quality
statements - publish that updated evidence
- three months later eg call from staff highlighting concerns – CQC review those
- follow up with registered manager
- further evidence gathering eg against three relevant quality statements
- publish findings and update ratings
- call to review progress with registered manager
34 quality statements – have a look here:
Key questions and quality statements – Care Quality Commission
Always remember though – the Fundamental Standards of Care, as set out in the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014 have not changed. The way in which CQC assess you against those Regulations will change, but the underlying requires are the same. If you’d like more information or bespoke training on the Fundamental Standards, we have fixed price half day training sessions available.
What is it?
The Court of Protection is a specialist court, established under the Mental Capacity Act 2005. Its primary role is to make decisions on financial or welfare matters for people who cannot make their own decisions, at the time they need to be made.
The jurisdiction of the Court of Protection can only be exercised when an individual is deemed to lack capacity.
Powers of the Court of Protection
The powers of the Court of Protection are wide ranging.
By way of two primary powers, the Court of Protection can:
- Make declarations such as whether an individual lacks capacity, or the lawfulness of an act, or an act yet to be done in relation to that individual
- Make decisions such as in relation to an individual’s welfare, care and treatment or finances
By way of further, non-exhaustive powers the Court of Protection can also make decisions to appoint of remove deputies and decide upon the validity of lasting powers of attorney.
When could you, as a social care provider be involved?
One or more of your service users may be the subject of Court of Protection proceedings, brought on their behalf by that individual’s Relevant Person’s Representative or Independent Mental Capacity Advocate.
As a social care provider, your involvement in Court of Protection cases may be formal or informal, varying from the following non-exhaustive list of examples:
- application of the Mental Capacity Act 2005 and code of practice capacity assessments and best interests decisions
- compliance with Third Party Disclosure Orders
- assessments for prospective admissions and identifying if care needs can be met
- attendance at round table meetings
- facilitating visits by advocates and Litigation Friends (whether in person or remotely)
- deprivations of liberty
- reporting on Standard Authorisation conditions
- input on discharge and conveyance plans
- behavioural contracts
Considerations
Court of Protection proceedings have the best interests of the individual subject to the proceedings at its core.
Initial involvement by care providers is to assist the court and parties with information gathering. Ensuring notes and assessments (in particular capacity assessments and best interests decisions evidencing proper application of the MCA and code of practice) are
sufficiently detailed, clear, contemporaneous and easily accessible is key to being able to comply with requests in a timely manner.
Court of Protection proceedings are subject to what are known as Transparency Orders, prohibiting information from being disclosed to the public, such as the name of the individual, their family members or witnesses requiring care and consideration.
If you would like further information or to arrange bespoke training, please get in touch.
A year ago the Independent Care Group (iCG) was one of dozens of small local organisations representing care providers. It had an active and well-known chair in Mike Padgham, but a relatively small income and covered a limited area.
Today, that situation has started to transform. Its income has doubled, it is providing new services to its 200 members in North Yorkshire and is poised to extend the geographic area it covers. And, at a time when social care faces massive challenges with few quick wins available, it is raising its voice to represent the sector.
The initiative for change came from the Board, according to Nick Swash, the chief executive: there was a sense that there was an opportunity for the organisation to do more but uncertainty about what direction it should take. This coincided with Nick – an experienced senior manager who has worked in a number of sectors – joining a year ago.
He identified the need for scale for the organisation – to increase its voice and “clout”, it needed to both increase the membership and revenue. Increased turnover could come from a number of areas – getting more grants from councils; commercial activities; and membership fees – although there was limited scope to increase these for existing members.
One of the ways it has achieved this income growth is by setting up an affinity partnership scheme with a number of trusted partners, offering services to members which they may not have access to inhouse.
“The iCG has had a partnership approach with Hempsons for a long time and have run the iCG legal advice line,” he says. Hempsons is now the premier affinity partner, with members encouraged to make use of its expertise in social care legal matters.
“We really appreciate our quarterly meetings with Hempsons. They are extremely good at what they do – and they are very local for most of the members,” he adds.
Nick says members are typically small and medium-sized organisations, focused on providing excellent care. Affinity partners can offer support with everything from legal matters to purchasing goods.
“Our aim is to improve the efficiency, productivity and sustainability of social care providers” he says. But he also wants to educate the NHS about social care with some big gaps in understanding and modes of operations – not to mention the difference in scale between small social care providers and NHS trusts, which can have a turnover of £1bn or more.
The members’ hearts are in the job they do. That is part of the issue, because the government and the NHS do not understand that. “They assume they are always on a paid salary” he comments. In reality, many social care providers are just trying to get through financially with very little scope to attract investment as they are making very limited profits. “They are just thinking about today” he adds.
This change in direction for the organisation poses questions about what is the role for a membership organisation. Nick argues that in this situation the organisation has to take a lead and move in a direction which aligns with what is likely to happen in the social care market. The membership, he reasons, will follow.
But he acknowledges members will differ in their level of engagement and how much they want the organisation to change. “We are looking at creating committees with members on them who can engage with other members on the strategy for the organisation” he adds.
So far the new direction seems to be paying dividends. Work recently has included co-operating with North Yorkshire County Council on a ‘Fair Cost of Care’ exercise to identify what would be a reasonable amount to pay for care and engagement with integrated care systems, on behalf of members. The iCG is also launching its own magazine this autumn – “Making Care Matter”.
“We will keep adding services and revenue until we have either achieved our goals or run out of room,” he says.
The iCG plans to get involved in two key areas where members can struggle: i) providing training courses and helping them with recruitment, ii) where overseas recruitment could offer relief for those struggling to get staff on the ground, but it is also very challenging.
Many NHS trusts have recruited from overseas extensively – but they have the critical mass to approach this in a way which may not be feasible for small care homes looking for a handful of staff. “The cost is phenomenal – about £6,000 a head,” Nick comments. He envisages the iCG playing a major part in overseas recruitment, potentially identifying staff, getting them through all the formalities and then offering them a range of jobs to go to.
But he suggests there could be other savings for members through working more closely together on things like a shared payroll provider where they could benefit from economies of scale. “We can’t have 200 members all going in different directions,” he says.
But there are also opportunities to extend the geographical area the organisation covers. It was recently invited – by the regional alliance and other bodies – to start representing care providers in South Yorkshire. Providers in Rotherham and Doncaster are likely to follow and the organisation representing care providers in West Yorkshire is keen to explore closer ties.
Nick comments: “We want to be the care providers’ organisation for the North of England. Large areas of the north – such as Lancashire – have no similar organisation, meaning social care’s voice is absent or diluted.”
“We need people like our chair Mike Padgham to continue to put our voice out there. Social care has to get a much louder voice going forward. Otherwise it is divide and conquer,” Nick concludes.
Find out more about the iCG at independentcaregroup.co.uk
Having just bounced back from the challenges brought about by COVID-19, care home operators now have the challenges of an unstable economy to deal with. With the cost of living rising, energy bills rocketing and bank borrowing becoming more expensive, where does that leave the market of selling and buying care homes?
Care homes have generally proven to be robust assets that have performed well during economic downturns. An aging population, coupled with strong supply and demand should mean that there will continue to be a demand for people wanting to acquire care homes, even during these challenging times. Nevertheless, the current uncertainty is bound to unsettle both sellers and buyers and create challenges in the selling and buying process.
Things to look out for as a buyer
Most people looking to acquire a care home or to add to their existing portfolio of homes are likely to be seeking bank financing for their acquisition. As we are all aware from the headlines, the cost of bank borrowing is going up. Therefore, as a buyer, it is important to shop around and check the terms of the loan agreement with your lender, paying particular attention to interest payments (and whether they are fixed or variable), the term of the loan and early repayment charges.
With the rising burden of energy prices, it will be important to check what contractual arrangements the home you are purchasing has with utility providers. This will be an important aspect of your legal due diligence. In fact, now more than ever, it will be critical to sense check the home’s supply chain generally to ensure that, as a business, it is getting value for money. If, once you have taken over, you want to change suppliers for various things, you will need to understand whether that will be possible or whether you are tied into certain contracts for a particular length of time.
Things to look out for as a seller
As buyers will be approaching the market more cautiously, as a seller, you need to consider how that may impact your sale. For example, buyers are likely to negotiate harder on sale prices. In addition, they may take a more risk averse approach to the transaction and rather than pay the full amount for the home upfront on day one, they may try to negotiate an “earn-out”. This would mean that, whilst a large proportion of the overall amount is paid on day one, a part of it will be held back and will only be paid if the home maintains or increases its revenue after the sale. From a buyer’s perspective, this is a sensible way to mitigate the risk of the business performing poorly once the buyer has taken over. If, as a seller, you are willing to agree to such a structure, it will be important to ensure that the “earn-out” provisions are clear in the sale and purchase contract and that you have necessary clauses protecting you.
The Francis Inquiry (into events at Stafford Hospital) led to, amongst many other recommendations, the creation of the statutory duty of candour, coupled with a professionalduty on doctors and nurses and a director duty too.
The statutory duty was implemented in November 2014, so has been in place for eight years now and is a core component of the CQC fundamental standards, as set out in reg 20 of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014:
- Registered Persons must act in an open and transparent way
- As soon as reasonably practicable after becoming aware that a notifiable safety incident has occurred…you must:
a. notify….that the incident has occurred and
b. provide reasonable support
3. Notification….must:
a. be given in person…
b. provide an account….
c. advise …what further enquiries….are appropriate
d. include an apology and
e. be recorded in a written record which is kept securely….
How to comply? What and when to report
What is a notifiable safety incident? And when do I need to report it? And to whom?
Each service provider should have a duty of candour policy that details internal processes – who to report any untoward incident to (no matter how big or small) and then what process will be followed around speaking to the affected person or their family and what needs to be said.
There are two statutory definitions of a notifiable safety incident – one for healthcare bodies and one for everyone else.
For social care providers the definition is:
…any unintended or unexpected incident that occurred in respect of a service user during the provision of a regulated activity that, in the reasonable opinion of a health care professional:
a. appears to have resulted in:
(i) the death
(ii) an impairment of the sensory, motor or intellectual functions of the service user which has lasted, or is likely to last for a continuous period of at least 28 days
(iii) changes to the structure of the body
(iv) prolonged pain or prolonged psychological harm
(v) shortening of life expectancy OR
(b) requires treatment by a healthcare professional in order to prevent:
(i) the death of the service user
(ii) any injury to the service user which, if left untreated, would lead to one or more of the outcomes above
Many incidents, such as a death, a fall downstairs or out of bed will obviously be notifiable but what about accidental bruising due to walking into a table? Is it ‘just’ a bruise, or is the bruise a sign of someone being unsteady on their feet or someone trying to walk unaided? A general rule of thumb might be that if there is a need to complete a body map and record the bruise, then it may well be notifiable.
Who are we notifying?
Initially, internally as all staff members should be encouraged to be open and honest and report any issue, big or small, to their registered manager or team leader. Don’t go off shift without sharing an issue.
It is for the registered manager or senior management team in an organisation to make the decision as to whether an incident is a notifiable one pursuant to duty of candour and whether the formal reporting requirements are engaged. HOWEVER, it is good practice to treat every incident, however big or small, as reportable, to encourage openness and transparency with individuals and their families.
Who do we talk to?
The “relevant person” that might be P, the person you are supporting, or if they lack capacity, are under 16 or perhaps in hospital unconscious, then you need to speak with the person lawfully acting on their behalf. That might be a parent, spouse, partner, someone holding an LPA or the executor under a will. Take care to talk to the right person, to pitch the information at the right level and to be sincere in your apology. There might need to be a two stage approach, an initial call/meeting to explain what has happened, what you are doing to investigate and an apology that its occurred, followed up with a more detailed meeting when you have more to say.
The purpose of duty of candour is to encourage openness and transparency. It’s not about trying to avoid disclosure of any particular issue to an individual or their family, or avoid accepting liability. It’s about working with an individual or their family and holding your hands up and saying sorry when something doesn’t quite go to plan or support isn’t 100%, as this is likely to happen when people are supporting people. Recognising that, and working in partnership, builds strength.
What if we get it wrong?
Fines are not huge, but can have a big impact reputationally. Compliance with duty of candour is managed by CQC who can and will take action to prosecute for failure to fulfil that statutory duty. Fines to NHS trusts have been more common, ranging from £1,250 to £16,250 together with legal costs and often a victim surcharge.
A private hospital that withheld details from four patients about a particular surgeon was fined £5,000, ordered to pay £15,000 in costs and £120 per victim.
Recently, a care home was fined £3,300 for failure to share details of a fall in a timely manner. They were also required to pay £181 victim surcharge and £7,890.61 costs to CQC.
Prosecutions are matters of public record and appear in trade publications. The fact of a prosecution can also impact on a services CQC rating. A breach of regulations is a rating limiter that can mean an otherwise outstanding service might only be rated as “requires improvement”.
Hempsons can help
Our dedicated social care team are all very familiar with duty of candour and supporting providers through many issues – big or small. Use our 15 minute free advice line on 01423 724056 to speak to a solicitor if you have any concerns. Don’t accept an offer from CQC to pay a fixed penalty notice to avoid prosecution – speak to us first, so that we can support you through the process.
Regulation 12 – don’t be afraid, be aware
Hempsons partner Philippa Doyle takes a look at Regulation 12, a regulatory fundamental standard of care.
All CQC registered providers, from the biggest NHS foundation trust down to the smallest care home, GPs and dentists alike, are required to adhere to the CQC fundamental standards of care and even though CQC are in the process of rolling out their new inspection regime (and publishing new questions that they will be asking during the inspection process), the underlying regulations and standards that providers must adhere to have not changed.
Set out in Section 2 of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014, each and every regulation must be followed but Regulation 12 can have the biggest consequences, for both the people you support, and you as a provider, if you get it wrong.
Regulation 12(1) Care and treatment must be provided in a safe way for services users
Of course it must. It goes without saying. It’s why you work in a caring industry. But what does “provided in a safe way” actually mean and what are CQC looking for?
The regs set out nine requirements that a provider must do and again, note the use of the word “must” – there’s no discretion here, you can’t not do something because it doesn’t work well in your service or you’ve never done it before – going back to the precise wording of the regs, and making sure you can deliver against that wording, is what will help take your service up a notch with CQC and enhance the lives of the people you support along the way.
Regulation 12(2) sets out the things which a registered person must do to comply with that paragraph:
a. assessing the risks to the health and safety of service users of receiving the care and treatment – make sure your care plans and risk assessments are up to date
b. doing all that is reasonably practicable to mitigate any such risk – if there is a risk of falls, show how your care plans and risk assessments mitigate that risk and how staff are trained and aware
c. ensuring persons providing care or treatment have the necessary competence, skills and experience to do so safely – link to your recruitment and training plans – ensure staff are up to date with mandatory training – ensure references are followed up for new staff, that inductions are completed and supervisions carried out
d. ensuring premises are safe for use and used in a safe way – daily/weekly visual checks and actioning loose treads on a stairway, splinters on a handrail, broken toilet seats
e. ensuring equipment used for providing care and treatment is safe for use and used in a safe way –even if provided by the LA direct to a patient, your staff still need to make sure it’s fit for purpose – is the inspection/safety certificate in date? Do a visual check before use each time (and document that!) make sure all staff are trained – eg hoists can differ – make sure new staff are trained on your hoists in the right way
f. where equipment or medicines are supplied by you, make sure there are sufficient quantities to ensure the safety of the service user and meet their needs – eg PPE, creams – don’t let stocks run out, ensure timely re-ordering
g. the proper and safe management of medicines – I can’t stress enough how important it is to ensure MAR charts are properly completed, audited and any gaps identified and rectified
h. assessing the risk and preventing, detecting and controlling the spread of infections, including those that are health care associated – ensure adequate PPE, ensure staff are trained, ensure staff use it. Encourage staff and service users to whistle-blow on anyone who doesn’t and take immediate action
i. where responsibility for care is shared with, or transferred to, other persons working with such other persons, service users and other appropriate persons to ensure that timely care planning takes place to ensure the health, safety and welfare of the service users – be very clear on who is responsible for what, ensure information is shared eg between GP, district nurses, care team – lack of communication is the biggest risk to provider, staff and service user in a shared care arrangement
Good record keeping, documentation, evidence and auditing are all at the heart of safe care and treatment. Know what your client needs, and ensure you deliver against it, and can evidence that you’ve delivered against it, every time.
Everything set out above should be second nature in any service, but where providers often fall down is their risk assessments and being in a position to demonstrate that you know your service users as well as you say you do, and that you’re delivering the care they are entitled to.
What happens if it goes wrong?
It’s not always about getting it wrong, as opposed to how you react to the situation. Any service involving people will sometimes have mishaps – even the most safely supported person can slip in the shower or a GP referral can be overlooked. The key is identifying the issue and responding to it in a timely way. CQC look to see how responsive you as a provider are to a situation. Did your systems and processes pick up the missed medication? Did your staff spot the missed medication and call the GP to check the impact on the patient? Or did you do nothing and gloss over it because the patient looks fine?
Sometimes things can go really wrong, and someone might die. Was that death inevitable, or did your service miss something? Did your systems and processes allow someone to fall through the gaps? Did you think one service was doing something in a shared care arrangement and they thought you were doing it?
CQC can and do prosecute for failure to deliver safe care and treatment. There will undoubtedly be an inquest. The police will investigate. They might not prosecute but CQC will pick up where the police left off and will often take action, even if the police don’t. It can take up to three years to get to that point and fines can be significant. Prosecution takes place in the magistrates court and fines reflect the size and turnover of your company. They are designed to be painful but not put you out of business, but we see weekly reports of care homes fines anywhere from £3,000 to £30,000 and more for avoidable deaths of care home residents. The NHS has seen fines much larger, where a patient in a mental health unit has managed to gain access to a roof and take their own life.
Don’t be afraid, be aware. Safe care and treatment benefits everyone.
What every charity and social enterprise employer should know
The Public Interest Disclosure Act protects workers, who report malpractice, from detriment or dismissal. The types of concern that can give rise to whistleblowing are issues which are close to the hearts of many charities and social enterprises, such as safeguarding, physical and financial abuse, and fraud. Nevertheless, awareness of whistle-blower protection among trustees and management is not always as high as it should be. This is a cause for concern, given that the number of whistleblowing claims brought in employment tribunals has grown year on year and at a faster rate than tribunal claims in general. Furthermore, there is anecdotal evidence of whistleblowing claims increasing as a result of the COVID-19 pandemic, especially in relation to staffing levels and PPE.
There is no financial cap on the compensation that can be awarded by employment tribunals in whistleblowing cases, and no requirement for a claimant to have minimum period of service to bring a claim. This makes whistleblowing particularly attractive for would be litigants, even where the link between the disclosure and their complaint appears tenuous.
There are two levels of protection for whistle-blowers, claims for which can be brought in an employment tribunal:
- dismissal of an employee for the reason, or principal reason, of being a whistle-blower is automatically unfair
- subjecting a worker to any detriment on the ground that they have made a protected disclosure is prohibited
The definition of “worker” for whistleblowing purposes is relatively wide but neither volunteers, non-executive directors (NEDs) nor trustees qualify for whistle-blower protection unless they are also workers. This is difficult to square with the duty imposed on charity trustees to report concerns to the regulator under the Charity Commission’s serious incident reporting regime. The Charity Commission recognised the importance of encouraging disclosures from volunteers when it amended its policy in 2019 to begin accepting whistleblowing disclosures from volunteers, but that still gave them no statutory protection from detriment.
New EU legislation expanding protection to volunteers and trustees will not apply in the UK due to Brexit, but it is possible that whistleblowing protection will be similarly expanded here in the future.
Recognise when whistle-blower protection applies
Whistle-blowers qualify for protection if they make a qualifying disclosure of information about:
- criminal offences, including fraud
- breach of a legal obligation
- miscarriage of justice
- danger to health and safety, including safeguarding
- damage to the environment
- the deliberate concealing of information about any of the above
The categories of wrongdoing overlap to a certain extent and, taken as a whole, are extremely wide. The wrongdoing can be past, present, prospective or merely alleged. It may concern the conduct of the employer, an employee, or a third party.
To qualify for protection, a worker must have a reasonable belief that the information disclosed tends to show one of the six relevant failures listed above. They must also have a reasonable belief that the disclosure is in the public interest. Finally, the disclosure should be made via the appropriate channels – workers are expected to report using internal procedures initially or to the Charity Commission or another regulator. Wider disclosures, such as to the media, will only qualify in very limited cases.
Determining whether a particular disclosure meets the definition of a protected disclosure is not always straightforward, so it is inadvisable to ignore a disclosure on the basis that it does not meet the criteria.
There is no requirement for a whistle-blower to make the disclosure in good faith (ie altruistically) to gain protection. This means that a serial whistle-blower, or someone who raises a concern for reasons self-preservation or motivated by a grudge, is still protected.
A protected disclosure can be more difficult to recognise where it is raised informally or alongside other issues.
For example, an employee may raise concerns by way of a grievance (or as one aspect of a wider grievance). Contrary to misconceptions sometimes held by employers and managers, to benefit from whistle-blower protection, there is no requirement for an employee to follow their employer’s policy in raising the concern, to use terminology associated with whistleblowing or even to recognise that they are making a protected disclosure.
Don’t underestimate the extent of whistle-blower protection
If the criteria are fulfilled, then the disclosure is a “protected disclosure” which means the whistle-blower is protected from dismissal and detriment. That does not make them “bullet proof”; rather, it means that they can bring employment tribunal proceedings if they can make a connection between detrimental treatment and making the disclosure.
The detriment may be imposed by the employer itself or by a fellow worker and in the case of the latter, the employer will usually be held liable for the actions of its staff and agents acting with its authority, whether or not the detriment took place with the employer’s knowledge or approval. An employer would only have a defence to vicarious liability if it took all reasonable steps to prevent the detrimental treatment. To utilise that defence, it would be vital to be able to show that staff in general, and the person accused in particular, have received whistleblowing training. Comprehensive, regular training where attendance is recorded helps to foster a culture in which concerns are welcomed, but it also means that an employer is far more likely to be able to show that it has taken reasonable steps to prevent staff from subjecting colleagues to detriment.
Training should remind managers that fellow workers and managers can be named as respondents in employment tribunal proceedings and held personally liable for the detriment.
Be ready and receptive to deal with disclosures
Information gained from staff, volunteers and other stakeholders speaking up can be a highly effective means for charities and social enterprises to manage risk and improve services. Check your organisation is following best practice by:
- putting in place an easily accessible whistleblowing policy, or appropriate written procedure to deal with whistleblowing
- making clear that your policy and procedure apply to NEDs, trustees and volunteers (even though they do not benefit from legal protection), making clear that such individuals are expected and encouraged to raise concerns
- raising and maintaining awareness among staff of the policy
- developing a culture of openness and accountability where staff feel safe to make disclosures, know who to approach, and are confident that they will not face retaliation
- offering support to staff who raise concerns and keep them informed about action taken to address them
- providing training on raising and recognising concerns
- appointing a freedom to speak up guardian or whistleblowing champion to encourage raising concerns and provide confidential advice and support to whistle-blowers
- reporting concerns to the Charity Commission where appropriate
Sources of further information
The Whistleblowing Commission, established in 2013 by the charity Public Concern at Work (now known as Protect) has produced a Whistleblowing Code of Practice which sets out best practice for whistleblowing policies, appropriate training in handling whistleblowing complaints and review and monitoring of whistleblowing in the workplace.
In March 2015, BEIS published Whistleblowing: Guidance for Employers and Code of Practice which explains employers’ responsibilities with regard to employees who blow the whistle.
NCVO has a range of resources and case studies aimed at charities on their website.



